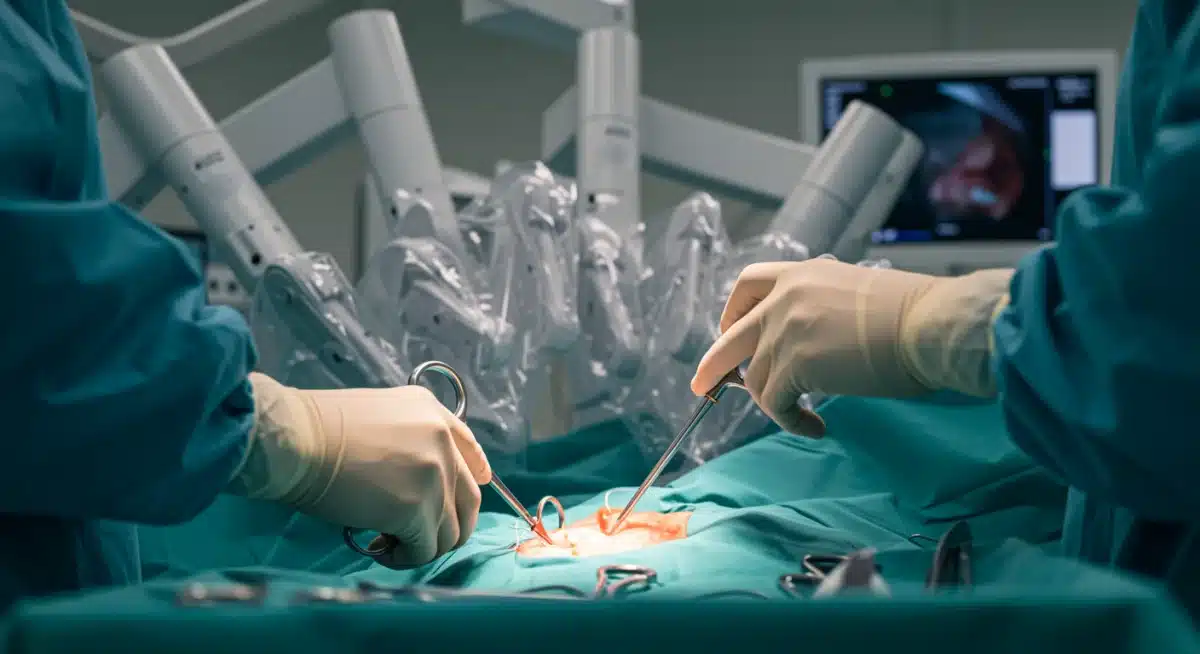
AI Robotic Surgery: 40% Faster Recovery in US Hospitals

AI-powered robotic surgery is revolutionizing patient care, significantly decreasing recovery times by 40% in U.S. hospitals this year, marking a pivotal moment in medical advancement.
The landscape of modern medicine is undergoing a profound transformation, with artificial intelligence (AI) at the forefront. Specifically, the integration of AI-powered robotic surgery is decreasing recovery times by 40% in U.S. hospitals this year, a statistic that underscores a monumental shift in how surgical procedures are performed and how patients heal. This isn’t just about technological sophistication; it’s about a tangible improvement in patient outcomes, reducing the burden of hospitalization, and accelerating the return to normalcy for countless individuals.
The dawn of AI in surgical precision
The introduction of AI into robotic surgery marks a new era of precision and efficacy that was once unimaginable. These systems go beyond mere automation; they learn, adapt, and assist surgeons with an unprecedented level of detail, leading to significantly better results.
AI algorithms analyze vast datasets of patient information, surgical techniques, and outcomes to provide real-time insights during operations. This data-driven approach enhances a surgeon’s capabilities, allowing for micro-level adjustments that human perception alone might miss. The intelligence embedded within these robots contributes directly to the reduction in invasiveness and trauma, which are key factors in faster recovery.
Enhanced visualization and navigation
One of the most immediate benefits of AI in robotic surgery is the superior visualization it offers. Surgeons gain access to high-definition, 3D views of the surgical site, often magnified many times over.
- Unparalleled clarity: AI enhances image processing, filtering out noise and highlighting critical anatomical structures.
- Real-time mapping: Advanced AI can create real-time maps of the surgical area, integrating pre-operative scans with live imaging.
- Augmented reality overlays: Some systems project crucial data directly onto the surgeon’s view, such as nerve pathways or tumor margins.
These capabilities allow surgeons to navigate complex anatomies with greater confidence and accuracy, minimizing damage to surrounding healthy tissues. The result is less bleeding, reduced pain post-operation, and a quicker healing process for the patient.
In essence, AI doesn’t replace the surgeon but augments their abilities, turning an already skilled hand into an even more precise instrument. This collaborative approach between human expertise and artificial intelligence is fundamental to the impressive reduction in patient recovery times observed across U.S. hospitals.
How AI-powered robots minimize surgical trauma
Minimizing surgical trauma is paramount for accelerating patient recovery, and AI-powered robotic systems excel in this area. Traditional open surgeries often involve large incisions, leading to significant tissue damage, blood loss, and prolonged healing. Robotic surgery, guided by AI, drastically alters this paradigm.
These sophisticated machines utilize tiny instruments inserted through small incisions, sometimes no larger than a keyhole. The AI component optimizes the movements of these instruments, ensuring they are as gentle and efficient as possible. This approach significantly reduces the physical toll on the patient’s body, which is a direct contributor to the 40% reduction in recovery times.
Precision beyond human capability
AI algorithms allow robots to execute movements with a steadiness and precision that even the most skilled human hand cannot consistently achieve. Tremors are eliminated, and movements are scaled down, meaning a large movement by the surgeon at the console translates to a minute, precise movement by the robot.
- Micro-movements: Robots can perform intricate tasks with sub-millimeter accuracy.
- Steady hands: AI counteracts any natural hand tremors of the surgeon, ensuring smooth operation.
- Optimal angles: Robotic arms can articulate in ways human hands cannot, reaching difficult areas with ease.
This extreme precision reduces the risk of accidental damage to nerves, blood vessels, and other delicate structures. When less surrounding tissue is disturbed, the body can focus its energy on healing the primary surgical site, rather than repairing widespread trauma.
Furthermore, AI can predict and mitigate potential complications by continuously analyzing physiological data during surgery. It can alert the surgical team to subtle changes that might indicate a problem, allowing for immediate intervention. This proactive approach prevents issues that could otherwise extend recovery, solidifying the role of AI in improving post-operative outcomes.
The impact on post-operative pain and complications
One of the most significant benefits of AI-powered robotic surgery, directly contributing to faster recovery, is the substantial reduction in post-operative pain and complications. Patients undergoing minimally invasive robotic procedures typically experience less discomfort compared to those undergoing traditional open surgery.
This decrease in pain is primarily due to the smaller incisions and reduced tissue manipulation. Less trauma to the body means less inflammation, which translates to less pain and a decreased reliance on strong pain medications. The ability to manage pain effectively is crucial for early mobilization and a smoother, quicker return to daily activities.
Fewer complications, faster healing
AI’s precision also plays a critical role in lowering the incidence of post-operative complications. By minimizing blood loss and reducing the risk of infection, patients are less likely to face setbacks that could prolong their hospital stay and recovery period.
- Reduced blood loss: Precise cuts and cauterization minimize bleeding, lowering the need for transfusions.
- Lower infection rates: Smaller incisions expose less internal tissue to the external environment, reducing infection risk.
- Decreased scarring: Smaller incisions lead to less visible scarring, which is not only cosmetic but also indicates less internal tissue disruption.
Moreover, AI can monitor patient vital signs and surgical parameters in real-time, identifying potential issues before they escalate. For instance, if a patient’s heart rate or blood pressure shows an unusual pattern, the AI can alert the surgical team, enabling them to address the issue promptly. This proactive monitoring is invaluable in preventing complications that could otherwise extend recovery, reinforcing AI’s transformative impact on patient care.
Accelerating patient mobilization and discharge
The ultimate goal of reduced recovery times is to enable patients to return home and resume their normal lives as quickly and safely as possible. AI-powered robotic surgery directly contributes to accelerating patient mobilization and discharge from hospitals, a key factor in the reported 40% reduction in recovery periods.
With less pain and fewer complications, patients are often able to get out of bed and move around much sooner after a robotic procedure. Early mobilization is not just about comfort; it’s a critical component of recovery, helping to prevent complications like deep vein thrombosis and promoting overall healing. The decreased need for extensive post-operative care also means patients can transition from hospital to home more swiftly.
Reduced hospital stays and costs
Shorter hospital stays are a direct consequence of faster recovery. This not only benefits the patient by reducing the risk of hospital-acquired infections and accelerating their return to a familiar environment but also has significant economic advantages for healthcare systems.
- Decreased length of stay: Patients typically spend fewer days in the hospital, freeing up beds.
- Lower healthcare costs: Reduced hospitalization translates to substantial savings for both patients and healthcare providers.
- Improved patient satisfaction: A quicker return home often leads to higher patient satisfaction with their surgical experience.
The efficiency gained through AI-powered robotic surgery allows hospitals to optimize resource allocation, serving more patients and improving overall operational capacity. This ripple effect extends beyond individual patient care, impacting the broader healthcare ecosystem by making high-quality surgical care more accessible and sustainable. The ability for patients to recover at home, often with minimal assistance, underscores the profound benefits of this technological integration.
Training and adoption in U.S. hospitals
The widespread adoption of AI-powered robotic surgery in U.S. hospitals is a testament to its proven benefits, but it also necessitates rigorous training and a strategic implementation approach. Surgeons and medical staff must undergo specialized training to effectively operate and manage these advanced systems.
This training typically involves a combination of simulation, hands-on practice with robotic systems, and supervised surgical procedures. Hospitals are investing heavily in these programs to ensure their teams are proficient, thereby maximizing the safety and efficacy of robotic surgery. The commitment to training is crucial for realizing the full potential of these technologies, including the 40% reduction in recovery times.
Overcoming implementation challenges
While the advantages are clear, integrating AI-powered robotic surgery into hospital workflows presents its own set of challenges. These include the significant upfront investment in equipment, the need for dedicated operating room space, and the continuous education of staff.
- Capital expenditure: Robotic systems represent a substantial financial commitment for hospitals.
- Staff training and re-training: Continuous education is required to keep pace with technological advancements.
- Workflow integration: Adapting existing surgical protocols to incorporate robotic systems requires careful planning.
Despite these hurdles, the long-term benefits, such as improved patient outcomes, reduced readmission rates, and enhanced hospital reputation, often outweigh the initial challenges. Many institutions are finding that the efficiencies gained and the improved quality of care justify the investment, positioning them at the forefront of medical innovation. The journey towards full integration is ongoing, but the trajectory clearly points towards a future where AI-powered robotic surgery is a standard of care.
The future outlook: continuous innovation and broader applications
The current achievements of AI-powered robotic surgery, particularly the 40% decrease in patient recovery times, are merely a glimpse into a future brimming with potential. Continuous innovation in AI and robotics promises even more sophisticated systems, expanding their applications across a wider spectrum of medical procedures and specialties.
Researchers are actively developing robots that can perform even more complex and delicate tasks, including micro-surgery and procedures within highly sensitive areas like the brain and spinal cord. The integration of haptic feedback, allowing surgeons to ‘feel’ tissues through the robotic instruments, is also advancing rapidly, further enhancing precision and safety. This ongoing evolution suggests that the benefits seen today will only multiply in the coming years.
Expanding surgical horizons
Beyond current applications, AI is poised to unlock new possibilities in surgical interventions. Personalized medicine, where AI tailors surgical plans to each patient’s unique anatomy and genetic profile, is becoming a reality.
- Personalized surgical planning: AI analyzes individual patient data to create custom surgical strategies.
- Predictive analytics: AI can predict surgical outcomes and potential risks with greater accuracy.
- Remote surgery: Advances in robotics and connectivity could enable surgeons to perform operations from distant locations, increasing access to specialized care.
The development of smaller, more agile robots will also allow for even less invasive procedures, potentially leading to outpatient surgeries for conditions that currently require hospital stays. Furthermore, AI’s role in pre-operative planning and post-operative monitoring will continue to grow, providing a holistic approach to patient care that optimizes every stage of the surgical journey. The trajectory of AI in robotic surgery is one of relentless progress, promising a healthier, more efficient future for healthcare.
| Key Aspect | Impact on Recovery |
|---|---|
| Surgical Precision | Minimizes tissue damage, leading to less pain and faster healing. |
| Reduced Trauma | Smaller incisions, less blood loss, and lower infection risk. |
| Post-operative Care | Decreased pain, fewer complications, enabling earlier mobilization. |
| Hospital Efficiency | Shorter hospital stays and optimized resource allocation. |
Frequently asked questions about AI robotic surgery
AI-powered robotic surgery involves using robotic systems enhanced with artificial intelligence to assist surgeons during operations. AI provides real-time data analysis, enhanced visualization, and precision movements, leading to more accurate and less invasive procedures. This technology significantly improves surgical outcomes and patient recovery.
AI robotic surgery reduces recovery times by enabling greater surgical precision, leading to smaller incisions, less tissue trauma, and reduced blood loss. This minimizes post-operative pain and complications, allowing patients to mobilize earlier and leave the hospital sooner, accelerating their overall healing process.
Yes, AI robotic surgery is considered safe. The AI augments the surgeon’s skills, providing enhanced control and precision, which can lead to fewer errors and complications compared to traditional methods. Rigorous training for surgical teams and continuous technological advancements further ensure patient safety during these procedures.
Many types of surgeries benefit, especially those requiring high precision in confined spaces. Common applications include prostatectomy, hysterectomy, cardiac procedures, and general surgeries like hernia repair. The technology is constantly expanding to new specialties, improving outcomes across a broad range of medical interventions.
The future of AI in robotic surgery involves continuous innovation, including more sophisticated algorithms for personalized surgical planning, enhanced haptic feedback, and the development of even smaller, more agile robots. Remote surgery capabilities and broader applications across micro-surgery and highly delicate procedures are also on the horizon.
Conclusion
The integration of AI into robotic surgery represents a monumental leap forward in healthcare, fundamentally reshaping patient care. The documented 40% reduction in recovery times in U.S. hospitals this year is a clear indicator of its transformative power, moving beyond theoretical promise to tangible, life-changing results. This evolution in surgical practice not only benefits individual patients through reduced pain, fewer complications, and faster returns to normal life but also optimizes healthcare resources, making advanced care more efficient and accessible. As technology continues to evolve, the collaborative synergy between human expertise and artificial intelligence will undoubtedly unlock even greater possibilities, solidifying AI-powered robotic surgery as a cornerstone of modern medicine.





