Generative AI in Medical Imaging 2026: 3-Month Outlook
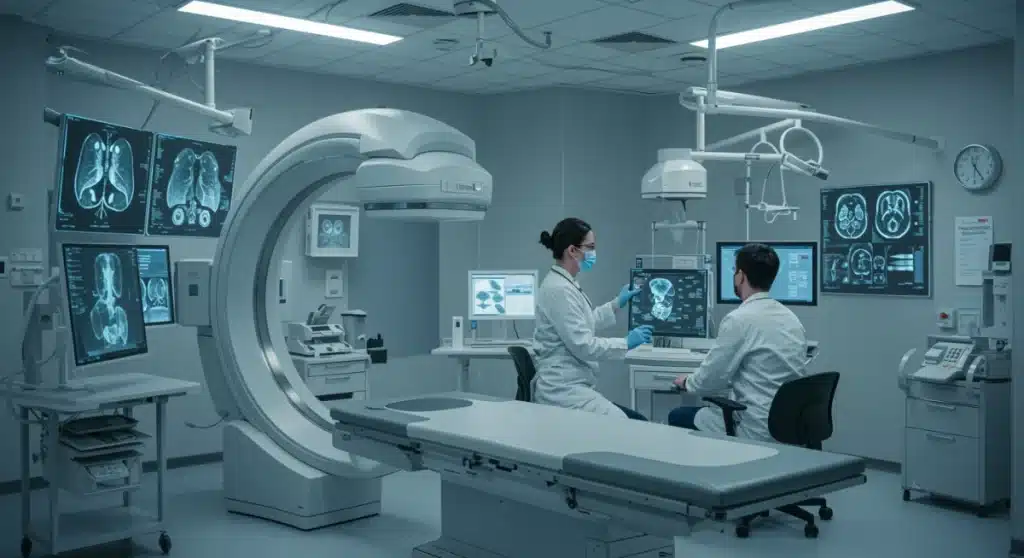
The immediate future of medical imaging in 2026 is poised for significant disruption by generative AI, promising enhanced diagnostic accuracy, streamlined workflows, and personalized patient care within a three-month horizon.
The landscape of healthcare is perpetually evolving, and by 2026, the integration of artificial intelligence, particularly generative AI, is no longer a distant concept but an immediate reality. We are on the cusp of witnessing how generative AI medical imaging will redefine diagnostics, treatment planning, and patient outcomes within just three months. This article delves into the transformative shifts anticipated and already underway.
The Immediate Horizon: Enhanced Diagnostic Capabilities
Generative AI’s most profound immediate impact on medical imaging lies in its ability to augment diagnostic capabilities significantly. Within the next three months, we expect to see tangible advancements in how radiologists and clinicians interpret complex medical images, leading to earlier and more accurate disease detection.
This rapid evolution is driven by AI models that can synthesize vast amounts of data, identifying subtle patterns that might elude the human eye. The precision offered by these systems is not just an incremental improvement but a fundamental shift in diagnostic paradigms.
Accelerated Anomaly Detection
Generative AI algorithms are becoming exceptionally adept at spotting anomalies in scans such as X-rays, MRIs, and CTs. Their training on massive datasets allows them to recognize even the most minute deviations from normal tissue structures, often before they become clinically significant.
- Early cancer detection in mammography and lung scans.
- Identification of subtle neurological changes in MRI, indicative of early-stage diseases.
- Detection of cardiovascular issues from imaging data.
Improved Image Reconstruction
Another critical area of impact is in image reconstruction. Generative AI can take low-resolution or incomplete scan data and reconstruct high-fidelity images, reducing scan times and patient exposure to radiation while maintaining diagnostic quality.
This capability is particularly valuable in emergency settings or for vulnerable patient populations, where quick and efficient imaging is paramount. The quality of these AI-enhanced reconstructions is often superior to traditional methods, offering clearer insights for diagnosis.
In summary, the enhanced diagnostic capabilities powered by generative AI represent a significant leap forward. Over the next three months, clinicians will increasingly rely on these tools to improve the speed and accuracy of their diagnoses, ultimately benefiting patient care.
Streamlining Workflows and Operational Efficiency
Beyond direct diagnostic improvements, generative AI is set to revolutionize operational workflows within medical imaging departments. The efficiency gains expected over the next quarter are substantial, addressing long-standing challenges related to workload, resource allocation, and reporting.
By automating repetitive tasks and optimizing image processing, generative AI frees up valuable time for radiologists and technicians, allowing them to focus on more complex cases and patient interaction. This shift not only improves productivity but also reduces burnout among healthcare professionals.
Automated Image Analysis and Prioritization
AI algorithms can automatically analyze incoming scans, flagging critical findings and prioritizing cases that require immediate attention. This intelligent triage system ensures that urgent conditions are addressed promptly, potentially saving lives.
The ability to handle a high volume of images with consistent accuracy is a game-changer for busy imaging centers. This automation extends to basic measurements and quantitative analyses, providing clinicians with objective data points for diagnosis.
- Automated measurement of tumor size and growth.
- Quantification of tissue density and organ volumes.
- Prioritization of scans showing acute conditions like strokes or fractures.
Intelligent Report Generation
Generative AI can assist in drafting preliminary radiology reports by extracting key findings from images and structuring them into coherent narratives. While human oversight remains crucial, this significantly accelerates the reporting process.
These AI-generated drafts can include standardized terminology and even suggest differential diagnoses, providing a solid foundation for radiologists to build upon. The consistency and speed of report generation improve communication within the healthcare team and expedite treatment decisions.
The streamlining of workflows through generative AI is poised to enhance the overall efficiency of medical imaging departments, ensuring that resources are optimally utilized and patient care is delivered more effectively and without undue delay.
Personalized Treatment Planning and Patient Care
The impact of generative AI extends beyond diagnosis and efficiency, reaching into the realm of personalized medicine. Within the next three months, we anticipate seeing how these advanced AI models contribute to highly individualized treatment plans and more empathetic patient care strategies.
By analyzing a patient’s unique imaging data in conjunction with other clinical information, generative AI can predict responses to various treatments, helping clinicians tailor interventions for optimal outcomes. This level of personalization represents a significant advancement over one-size-fits-all approaches.
Predictive Modeling for Treatment Response
Generative AI can create predictive models based on a patient’s specific imaging biomarkers, forecasting how a tumor might respond to chemotherapy or radiation therapy, or how a heart condition might progress. This allows for proactive adjustments to treatment regimens.
The ability to simulate various treatment scenarios based on an individual’s data empowers both clinicians and patients to make more informed decisions, leading to more effective and less burdensome therapeutic pathways.
- Forecasting tumor regression rates with different drug combinations.
- Predicting the efficacy of surgical interventions based on anatomical variations.
- Personalizing radiation dosages to minimize side effects while maximizing therapeutic impact.
Enhanced Patient Communication and Education
Generative AI can also create personalized visual aids and explanations derived from a patient’s own scans. This helps patients better understand their condition, the proposed treatment, and potential outcomes, fostering greater engagement and adherence.
Imagine a patient seeing a 3D model of their own anatomy, highlighting the area of concern and how a proposed treatment would affect it. This visual clarity can significantly reduce anxiety and improve patient comprehension.
In essence, generative AI is paving the way for a more personalized and patient-centric approach to healthcare. The next three months will showcase its growing role in crafting bespoke treatment plans and improving the overall patient experience.
Challenges and Ethical Considerations in the Short Term
While the promise of generative AI in medical imaging is immense, its rapid deployment over the next three months also brings significant challenges and ethical considerations that must be addressed. Navigating these complexities will be crucial for its successful and responsible integration into healthcare.
Issues such as data privacy, algorithmic bias, and the need for robust regulatory frameworks are at the forefront. Stakeholders must collaborate to ensure that the benefits of AI are realized without compromising patient safety or trust.
Data Privacy and Security
The use of vast amounts of patient imaging data for AI training and application raises critical concerns about privacy and security. Protecting sensitive health information from breaches and misuse is paramount.
Robust encryption, anonymization techniques, and secure data governance policies are essential to maintain patient trust and comply with regulations like HIPAA. The rapid pace of AI development necessitates equally rapid advancements in data protection.
Addressing Algorithmic Bias
Generative AI models are only as unbiased as the data they are trained on. If training datasets disproportionately represent certain demographics, the AI may perform less accurately or even generate biased outcomes for underrepresented groups.

Ensuring diverse and representative datasets is crucial to developing equitable AI systems. Ongoing monitoring and validation of AI performance across different patient populations are necessary to identify and mitigate bias.
- Ensuring AI models are trained on diverse demographic data.
- Regular auditing of AI outputs for fairness and accuracy.
- Developing transparent AI models to understand their decision-making processes.
Over the next three months, the healthcare industry will grapple with these challenges, working towards solutions that enable the safe, ethical, and equitable implementation of generative AI in medical imaging.
Regulatory Landscape and Industry Standards by 2026
As generative AI rapidly integrates into medical imaging, the regulatory landscape is scrambling to keep pace. By 2026, we anticipate a more defined, though still evolving, set of guidelines and industry standards aimed at ensuring the safety, efficacy, and accountability of these advanced AI systems.
Regulatory bodies like the FDA in the United States are actively working on frameworks that balance innovation with patient protection. The next three months will likely see further clarification and perhaps even new mandates regarding AI-powered medical devices and software.
FDA Approvals and Guidelines
The FDA has already begun approving AI-powered medical devices, and this trend will accelerate. However, generative AI’s dynamic nature, with its ability to continuously learn and adapt, presents unique challenges for traditional regulatory pathways.
We expect to see more specific guidance on how AI models are validated, how their performance is monitored post-market, and what level of transparency is required from developers. The emphasis will be on ensuring that AI systems remain safe and effective throughout their lifecycle.
- Clearer pathways for AI software as a medical device (SaMD) approvals.
- Guidelines for continuous learning AI systems and their re-validation.
- Increased scrutiny on data provenance and model robustness.
Industry Best Practices and Standardization
Beyond government regulations, industry organizations and professional bodies are developing best practices and standards for the responsible use of generative AI in medical imaging. These include recommendations for data handling, model development, and clinical integration.
The aim is to foster a collaborative environment where innovation thrives while maintaining high ethical and quality standards. Standardization will be key to ensuring interoperability and widespread adoption across different healthcare systems.
The regulatory and industry standard landscape for generative AI in medical imaging is dynamic. The coming three months will be critical in shaping the frameworks that will govern the ethical and effective deployment of these powerful technologies, ensuring they serve humanity responsibly.
The Human Element: Radiologists and AI Collaboration
Contrary to fears of displacement, the immediate future of generative AI in medical imaging, particularly within the next three months, points towards a powerful collaboration between human radiologists and intelligent machines. AI is not replacing radiologists but augmenting their capabilities, transforming their roles into more strategic and analytical ones.
This symbiotic relationship leverages the strengths of both parties: the AI’s speed and pattern recognition, and the radiologist’s nuanced understanding, clinical judgment, and empathetic patient care. The focus shifts from rote image interpretation to complex decision-making and patient management.
Augmented Intelligence, Not Artificial Replacement
Generative AI tools are best viewed as advanced assistants, providing radiologists with deeper insights, second opinions, and automated preliminary analyses. This ‘augmented intelligence’ approach enhances diagnostic accuracy and reduces cognitive load.
Radiologists can focus on interpreting the most challenging cases, communicating findings to clinicians, and engaging in patient consultations, tasks that require uniquely human skills and empathy. The AI handles the heavy lifting of initial screening and quantitative analysis.
- AI highlighting suspicious regions for radiologist review.
- Providing quantitative metrics to support diagnostic decisions.
- Automating routine tasks, freeing up radiologist time.
Training and Adaptation for Healthcare Professionals
The rapid integration of generative AI necessitates new training and adaptation for current and future radiologists. Educational programs are already incorporating AI literacy, focusing on how to effectively use, validate, and troubleshoot AI tools.
Over the next three months, we will see an increased emphasis on upskilling healthcare professionals to leverage these technologies, ensuring they are comfortable and proficient in working alongside AI. This adaptation is crucial for maximizing the benefits of AI integration.
Ultimately, the human element remains central to medical imaging. Generative AI will empower radiologists, enabling them to deliver more precise, efficient, and personalized care. The collaboration between humans and AI will define the next era of diagnostic medicine, solidifying the radiologist’s role as an indispensable expert.
| Key Impact Area | 3-Month Outlook |
|---|---|
| Diagnostic Accuracy | Significant improvements in early disease detection and anomaly identification. |
| Operational Efficiency | Streamlined workflows, automated reporting, and faster image processing. |
| Personalized Care | Enhanced treatment planning and patient education through individualized insights. |
| Ethical Considerations | Ongoing efforts to address data privacy, bias, and regulatory frameworks. |
Frequently Asked Questions About Generative AI in Medical Imaging
Generative AI is already rapidly integrating into medical imaging. Within the next three months, its presence will become more pronounced in advanced diagnostic tools, image reconstruction, and workflow automation, moving swiftly towards mainstream adoption in specialized centers.
No, generative AI is not expected to replace radiologists by 2026. Instead, it will serve as an indispensable assistant, augmenting radiologists’ capabilities by automating routine tasks, improving diagnostic accuracy, and allowing them to focus on complex cases and direct patient care.
The primary benefits include enhanced diagnostic accuracy for earlier detection, significant improvements in operational efficiency through automated workflows, and the ability to create more personalized treatment plans for patients, leading to better outcomes.
Key ethical challenges include ensuring data privacy and security of sensitive patient information, mitigating algorithmic bias to ensure equitable care across all demographics, and establishing clear regulatory frameworks for accountability and validation of AI systems.
Healthcare professionals, particularly radiologists, will undergo training to effectively utilize and interpret AI-generated insights. The adaptation will focus on collaborative workflows, where AI handles preliminary analysis, allowing human experts to apply critical judgment and clinical expertise.
Conclusion
The immediate outlook for generative AI medical imaging in 2026 is one of profound transformation and accelerated progress. Within the next three months, we are poised to witness tangible advancements that will redefine diagnostic processes, significantly enhance operational efficiencies, and pave the way for increasingly personalized patient care. While challenges related to data privacy, algorithmic bias, and regulatory frameworks persist, the concerted efforts of researchers, clinicians, and policymakers are aimed at ensuring a responsible and ethical integration of these powerful technologies. The future of medical imaging is undeniably collaborative, with generative AI serving as an invaluable partner to human expertise, ultimately leading to improved health outcomes and a more effective healthcare system.





