2026 FDA Approvals: Dominant AI Models in Healthcare
The landscape of healthcare in 2026 will be significantly shaped by FDA-approved AI models, predominantly in diagnostic imaging, personalized treatment recommendations, and accelerated drug discovery, offering unprecedented advancements in patient care and medical research.
As we advance toward 2026, the intersection of artificial intelligence and healthcare is becoming increasingly critical, particularly concerning regulatory oversight. The question of Navigating 2026 FDA Approvals: What AI Models in Healthcare Will Dominate? is not merely academic; it represents a pivotal shift in how medical solutions are developed, validated, and ultimately delivered to patients. This era promises a transformation in diagnostics, treatment, and patient management, driven by intelligent systems that learn and adapt.
The Evolving FDA Landscape for AI in Healthcare
The U.S. Food and Drug Administration (FDA) has been actively adapting its regulatory frameworks to accommodate the rapid pace of AI innovation in healthcare. Unlike traditional medical devices, AI models often learn and evolve, presenting unique challenges for pre-market approval and post-market surveillance. By 2026, the FDA’s approach is expected to be more streamlined, focusing on robust validation protocols that ensure safety, efficacy, and transparency.
This evolving landscape is not just about approving static software; it’s about establishing clear pathways for AI models that continuously improve. The FDA recognizes that AI’s dynamic nature requires a different regulatory paradigm, one that encourages innovation while safeguarding public health. Manufacturers are now tasked with demonstrating not only initial performance but also the reliability of their AI models over time, especially as they encounter new data.
Regulatory Frameworks and Predetermined Change Control Plans
A key development is the FDA’s emphasis on Predetermined Change Control Plans (PCCPs). These plans allow AI developers to specify modifications an AI algorithm can make without requiring a new 510(k) clearance or premarket approval (PMA) each time. This foresight is crucial for adaptive AI models.
- Transparency Requirements: Manufacturers must clearly articulate the intended use, data sources, and performance metrics of their AI models.
- Real-World Performance Monitoring: Post-market surveillance is becoming more rigorous, requiring continuous data collection and analysis to ensure ongoing efficacy and safety.
- Data Governance: Strict guidelines on data quality, bias detection, and algorithmic fairness are being established to prevent disparities in healthcare outcomes.
The FDA’s commitment to these evolving frameworks signals a maturation in how AI is viewed within the healthcare ecosystem. Companies that proactively integrate these regulatory considerations into their development lifecycle will be better positioned for successful approval by 2026. Understanding these nuances is paramount for any AI model aiming for market dominance.
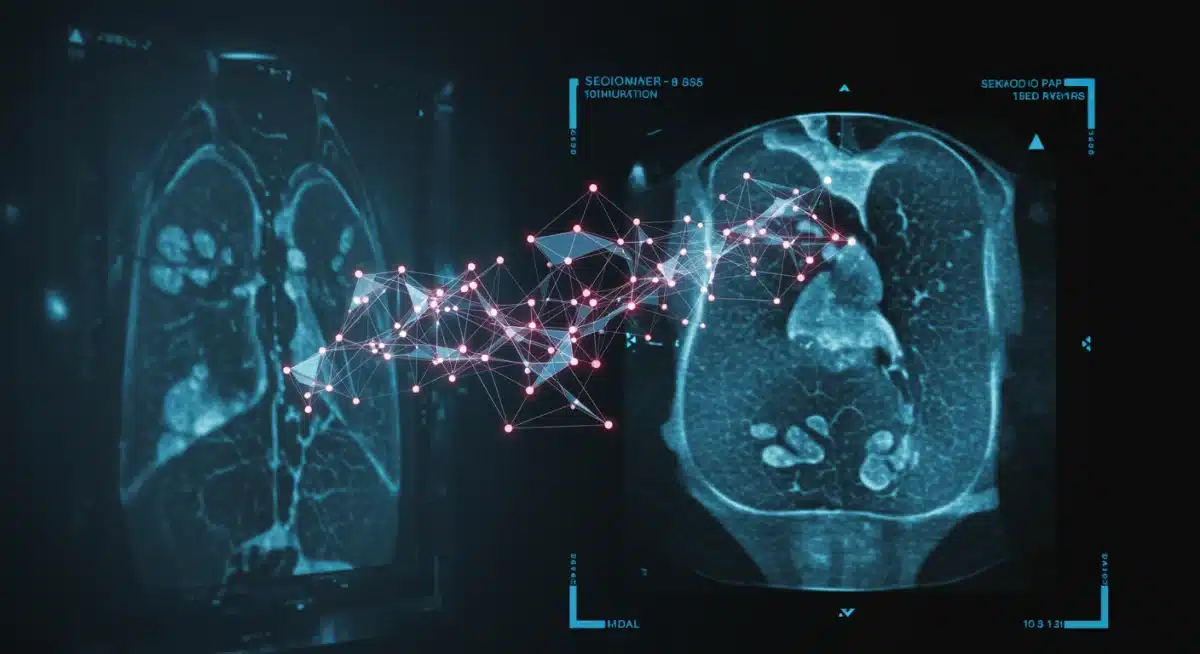
Diagnostic Imaging AI: Leading the Charge
One of the most prominent areas where AI models are expected to dominate FDA approvals by 2026 is diagnostic imaging. AI algorithms can analyze medical images—such as X-rays, MRIs, and CT scans—with remarkable speed and accuracy, often surpassing human capabilities in detecting subtle anomalies. This capability has profound implications for early disease detection and personalized treatment planning.
The sheer volume of imaging data generated annually is staggering, and radiologists face immense pressure to interpret these images efficiently and accurately. AI offers a powerful tool to augment their work, reducing burnout and improving diagnostic consistency. We anticipate a surge in approvals for AI models that assist in identifying cancerous lesions, cardiovascular diseases, and neurological conditions, among others.
Key Areas of Diagnostic Imaging AI Innovation
Several specialized areas within diagnostic imaging are ripe for AI-driven transformation and subsequent FDA approval. These include:
- Radiology: AI for automated detection of polyps in colonoscopies, lung nodules in CT scans, and breast cancer in mammograms.
- Pathology: AI-powered analysis of tissue samples to identify disease markers and grade tumor aggressiveness.
- Ophthalmology: AI systems for early detection of diabetic retinopathy, glaucoma, and macular degeneration from retinal scans.
These applications underscore AI’s potential to revolutionize how diagnoses are made, leading to earlier interventions and better patient outcomes. The FDA’s focus will be on validating the clinical utility and robustness of these systems across diverse patient populations, ensuring equitable access and reliable performance.
Personalized Medicine and AI-Driven Treatment Plans
The promise of personalized medicine—tailoring medical treatment to the individual characteristics of each patient—is being realized through advanced AI models. By 2026, we expect a significant number of FDA approvals for AI systems that analyze vast amounts of patient data, including genomics, electronic health records, and lifestyle factors, to recommend highly individualized treatment plans.
These AI models move beyond one-size-fits-all approaches, offering insights into drug efficacy, potential side effects, and optimal dosages based on a patient’s unique biological profile. This level of precision medicine has the potential to dramatically improve therapeutic outcomes, particularly in complex diseases like cancer and autoimmune disorders.
The regulatory challenge here lies in validating the safety and effectiveness of these highly individualized recommendations. The FDA will likely scrutinize the algorithms’ ability to handle diverse patient cohorts and ensure that biases in training data do not lead to inequitable treatment recommendations. Demonstrating a clear clinical benefit and a strong ethical framework will be crucial for approval.
Drug Discovery and Development Acceleration with AI
The traditional drug discovery process is famously long, expensive, and fraught with high failure rates. AI models are rapidly changing this paradigm, and by 2026, we anticipate several FDA approvals stemming from AI-accelerated drug discovery and development pipelines. These models can identify promising drug candidates, predict their efficacy and toxicity, and optimize clinical trial designs at an unprecedented pace.
AI’s ability to sift through massive chemical libraries, simulate molecular interactions, and identify novel therapeutic targets is transforming pharmaceutical research. This not only speeds up the time to market for new drugs but also reduces the financial burden, potentially making life-saving treatments more accessible.
Impact on Pharmaceutical Innovation
- Target Identification: AI algorithms can analyze biological pathways and disease mechanisms to pinpoint novel drug targets.
- Molecule Design and Optimization: Generative AI models can design new molecules with desired properties, reducing the need for extensive experimental screening.
- Clinical Trial Optimization: AI can help identify suitable patient populations, predict trial outcomes, and monitor patient responses, leading to more efficient and successful trials.
The FDA’s role in this domain will involve ensuring the rigor of the AI-driven discovery process and the validity of preclinical and clinical data generated. Companies leveraging AI in their drug development efforts will need to provide comprehensive documentation on the AI’s methodology, validation, and impact on the overall development timeline and success rates.
Ethical Considerations and AI Bias in Healthcare
As AI models become more integrated into healthcare, ethical considerations and the potential for algorithmic bias are paramount. The FDA, in its approval processes for 2026, will increasingly prioritize models that demonstrate fairness, transparency, and accountability. Bias in AI algorithms can lead to disparities in diagnosis or treatment for certain demographic groups, exacerbating existing health inequities.
Addressing these concerns requires robust data governance, diverse training datasets, and explainable AI (XAI) techniques that allow clinicians to understand how an AI model arrived at its conclusions. Manufacturers must not only prove efficacy but also demonstrate a proactive approach to mitigating bias throughout the AI lifecycle.
Mitigating Bias and Ensuring Fairness
Several strategies are being adopted to address AI bias and ethical concerns:
- Diverse Data Sets: Training AI models on data that represents a wide range of patient demographics, ethnicities, and socio-economic backgrounds.
- Algorithmic Audits: Regular independent audits of AI algorithms to detect and correct biases.
- Explainable AI (XAI): Developing AI systems that can articulate their reasoning, allowing clinicians to critically evaluate recommendations.
- Human-in-the-Loop: Ensuring that human oversight remains central to decision-making, with AI serving as a supportive tool rather than a replacement for clinical judgment.
The FDA’s regulatory framework will evolve to include specific requirements for bias assessment and mitigation, pushing developers to build more equitable and trustworthy AI systems. Models that prioritize these ethical considerations will gain a significant competitive advantage in the approval process.
The Future of AI in Healthcare: Beyond 2026 Approvals
While 2026 promises a wave of FDA approvals for AI models in diagnostics, personalized medicine, and drug discovery, the trajectory of AI in healthcare extends far beyond this immediate horizon. The innovations we see gaining traction now are merely stepping stones to a more integrated, predictive, and preventive healthcare system. Future AI models will likely focus on even more complex challenges, such as population health management, remote patient monitoring at scale, and the development of fully autonomous surgical robots.
The continuous evolution of AI technologies, coupled with advancements in data science and computational power, will unlock new possibilities that are currently unimaginable. The FDA’s role will remain crucial, adapting its oversight to ensure that these cutting-edge technologies are introduced safely and effectively, fostering an environment where innovation thrives responsibly.
Looking ahead, we can anticipate AI models that not only assist in clinical decisions but also proactively manage patient health, predict disease outbreaks, and even contribute to the development of novel therapeutic modalities like gene editing and regenerative medicine. The focus will shift from treating illness to maintaining wellness, with AI serving as the intelligent backbone of this transformation. The journey of AI in healthcare is just beginning, and 2026 is a significant milestone in its rapid progression.
| Key Focus Area | Description of Impact |
|---|---|
| Diagnostic Imaging AI | AI models enhancing accuracy and speed in interpreting medical images for early disease detection. |
| Personalized Medicine | AI systems tailoring treatments based on individual patient genomics and health data. |
| Drug Discovery Acceleration | AI models accelerating the identification, design, and optimization of new drug candidates. |
| Ethical AI & Bias Mitigation | Emphasis on fair, transparent AI models to prevent disparities and build trust. |
Frequently Asked Questions About 2026 FDA AI Approvals
Primary challenges include demonstrating continuous safety and efficacy for adaptive AI, ensuring transparency in algorithmic decision-making, addressing potential biases in training data, and developing robust post-market surveillance plans to monitor real-world performance over time.
The FDA is adapting by implementing Predetermined Change Control Plans (PCCPs), which allow for specified modifications to AI algorithms without repeated approvals. They also emphasize real-world performance monitoring and stringent data governance to ensure ongoing reliability.
AI applications in radiology for automated detection of anomalies like lung nodules and breast cancer, pathology for tissue analysis, and ophthalmology for early detection of eye diseases are expected to receive significant FDA approvals.
By 2026, AI will drive personalized medicine by analyzing extensive patient data, including genomics and health records, to recommend highly individualized treatment plans. This enhances precision in drug efficacy, dosage, and side effect prediction for complex diseases.
Ethical considerations are crucial, with the FDA prioritizing AI models that demonstrate fairness, transparency, and accountability. This includes mitigating algorithmic bias through diverse datasets, regular audits, and explainable AI techniques to prevent healthcare disparities.
Conclusion
The year 2026 stands as a landmark for AI in healthcare, particularly concerning FDA approvals. The models poised to dominate—from diagnostic imaging and personalized medicine to accelerated drug discovery—represent a profound evolution in medical science. The FDA’s adaptive regulatory approach, coupled with an increasing focus on ethical AI and bias mitigation, ensures that these powerful technologies are integrated responsibly. This period will undoubtedly set the stage for a future where AI not only supports but actively transforms healthcare delivery, making it more precise, efficient, and equitable for all.